🤔What is PHEM?
Pre-hospital emergency medicine is a sub-specialty closely tied to emergency medicine, intensive care medicine, and anesthetics. It aims to provide lifesaving medical care to patients in critical need, in order to stabilise them before transferring them to hospital.
🚑Key Responsibilities in the Field
The scenarios that doctors will attend are wide and varying, not only due to the array of medical conditions, but also due to the different locations and situations each patient presents in. The most common call outs include but are not limited to: cardiac arrests, trauma calls including road traffic accidents and falls, and medical emergencies such as anaphylaxis and status epilepticus.
As a result, the training pathway develops clinicians to excel in the following:
- Airway management and ventilatory support
- Resuscitation care; CPR and defibrillation
- Trauma care (haemorrhage control, neuroprotection, splinting fractures)
- Medical management of acute presentations
- Procedural skills such as arterial lines, emergency thoracotomy
- Covers all demographics, from children, pregnant mothers and elderly
- Assess human and geographical factors affecting provision of care
- Support rescue and extraction of patients
- Safely transfer patients to hospitals
Not only must doctors be able to do the above, but they must be able to do the above well. Having a solid base in these skills prior to PHEMS training is incredibly useful, as medics will have to battle against many uncontrollable factors whilst treating their patients, making the task much more challenging. For example, doing an arterial line in windy conditions at the top of a mountain where clinicians must find ways to overcome the logistical issue of equipment being blown away. This makes PHEMS unique in its constant variation of presentations, as no two cases are the same.

🚨A typical day in the life of a PHEMs trainee
5:00am-wake up
5:30am-morning preparation for the day ahaed
6:30am-arrive at base
7:00am-handover with pilots and clinicians in the debrief room
7:30am-kit checks; check the car and the kit in the boot, as well as checking the kit in the aircraft
8:00am-control drug check
8:45am-debrief with pilots regarding flight risk
9:00am-bag check; ensure that extra equipment is to hand if needed
9:30am onwards– await a call out, and in the meantime, facilitate charity visits or attend simulations to improve on efficiency and skills
19:00pm-home
Each day on site varies considerably, depending on the call outs received, and requires good communication skills and trust within teams, working closely with pilots, paramedics, and other doctors.
⚡How to pursue a career in PHEM
In 2011, a dedicated training pathway was created to ensure doctors are adequately trained to be able to carry out this high level of care. Due to the complexity of the specialty, only ST4 and above in select fields can be eligible for the PHEM pathway. It can be done as part of a pre-existing training programme or it can be done out-of-programme. Below, there is a diagram outlining the path into the formal PHEMs training pathway.
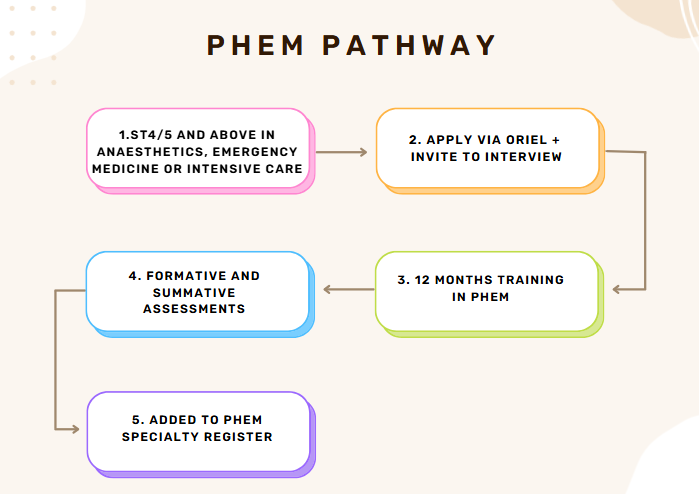
- Person specification is released, requiring a minimum of ST4 training at the time of application. Other experience is desirable, such as QIs in pre-hospital medicine, as well as pre-hospital skills training.
- Once the role is on Oriel, applicants can apply and rank their geographical preference. If invited, candidates are invited to an online interview day, where they are questioned on their portfolio and then asked to do a clinical scenario. Following this, successful applicants will then be required to do a fitness test, due to the physical nature of the job.
- Training lasts 12 months full-time or equivalent if part-time. During these months, there are 3 different phases of training that occur, taking a trainee from full supervision to working independently, and over time, the contact with the supervising consultant is reduced.
- Formative assessments
- In order to ensure adequate progression, as with all specialties, PHEM trainees must keep their portfolio up to date, using case-based discussions, mini-CEX or OSATS (observed shift assessment tool; special to PHEM, where a consultant assesses how a trainee performs throughout the course of a day)
- SIMS may also be used to assess competencies
5. Summative Assessments
- Trainees must pass 2 national exams, one at 6 months called Diploma in Immediate Medical Care (DIMC) and another at 12 months called the Fellowship in Immediate Medical Care (FIMC), which include single best answer questions, and an OSCE style exam component.
- Together these assessments feed into the final educational review and structured training report, which ultimately decide upon adequate completion of the training.
- Once added to the PHEM specialty register, doctors can become consultants in both PHEM and their base specialty after completing their primary training.
📌How to improve your portfolio
- Get involved in events or expedition medicine; join societies (e.g. wilderness medicine, emergency medicine) and volunteer at sporting events (particularly extreme sports and treks in remote areas) in order to gain exposure beyond the hospitals
- Whilst at university, it may be helpful to consider intercalating in a relevant subject area (i.e. Acute, Critical and Emergency Care or Remote medicine); for more information look at Intercalations: The Ultimate Guide – More than Medics
- Once ALS approved, work towards becoming an instructor of ILS/ALS
- If possible, do QI’s on prehospital medicine or on topics closely related to pre-hospital medicine
- Check the curriculum and ensure that you fit the specification; don’t treat it like a tick box exercise but aim to develop skills as a clinician too
- Doctors involved in the army may have an advantage due to the training provided, so this may be an alternative pathway for people to consider
- Check opportunities available at the different air ambulance organisations, St Johns ambulance and so on.
- Attend conferences linked to PHEM, such as BASICS, FPHC or RCEM.
- BASICS: A charity that provides courses, conferences and aid for those wanting to pursue a career within pre-hospital care.
- Take part in observerships and electives related to pre-hospital medicine.
- Ask to shadow paramedics to gain valuable pre-hospital care experience
⛑️Skills needed for a Career in PHEM
- Calm under pressure: able to make critical decisions quickly in chaotic or life-threatening situations.
- Excellent clinical judgment: confident managing acutely unwell or injured patients with limited resources.
- Strong teamwork and leadership: comfortable leading multi-agency teams (paramedics, fire, police, air ambulance crews).
- Adaptable and resourceful: can work in challenging environments (roadside, wilderness, or disaster scenes).
💭Why pursue a career in PHEM?
- Immediate, Life-Saving Impact: makes for a very fulfilling hands-on role, while making life or death decisions.
- Variety: No two scenarios are the same. You might respond by helicopter, ambulance, or rapid response car, and work in locations ranging from motorways to rural hillsides. The unpredictability keeps the job unique and dynamic.
- Meaningful and Rewarding Work: There’s a strong sense of purpose in knowing that the practical skills you apply directly contribute to saving lives and making an immediate difference in patient outcomes.
Resources and Useful Websites
- Institute for Pre-hospital Emergency Medicine
- The Intercollegiate Board for Training in Pre-Hospital Emergency Medicine
- Subspeciality training in PHEM Guide
- The applicants guide to PHEM
- FICM: PHEM article
- Qualification in Emergency Response Ambulance Driving
- Qualification in Immediate response Emergency Care
- How to become an Emergency Medical Technician

Reviewed by Dr Felipe Urriola-Perez
A special thanks to Dr Felipe Urriola-Perez (PHEM fellow at LNAA) who provided valuable insight into this article





